h pylori and probiotics
 Are probiotics useful for therapy of Helicobacter pylori diseases? - ScienceDirect
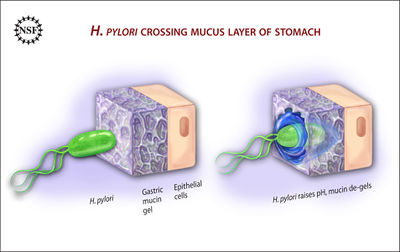
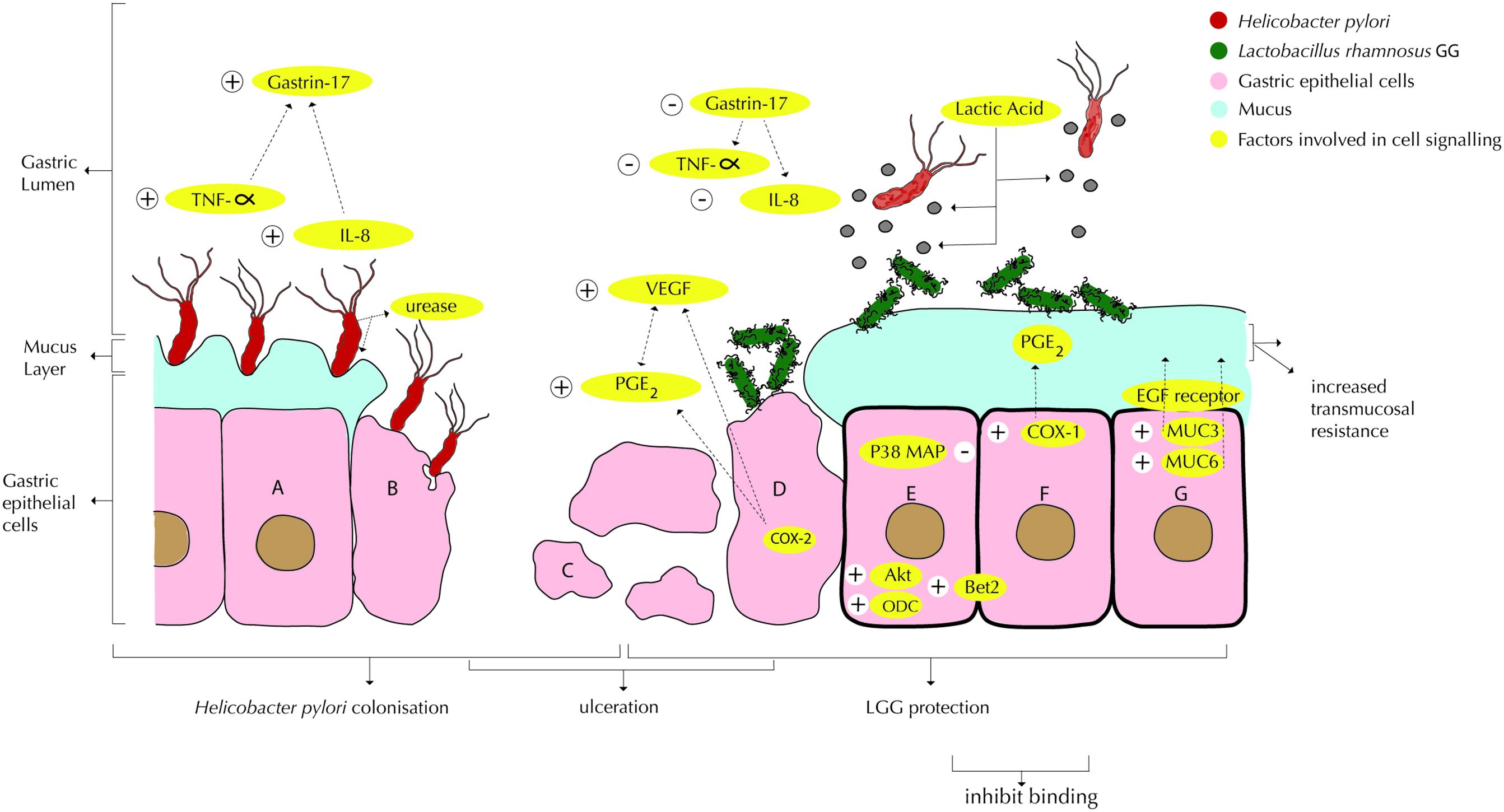
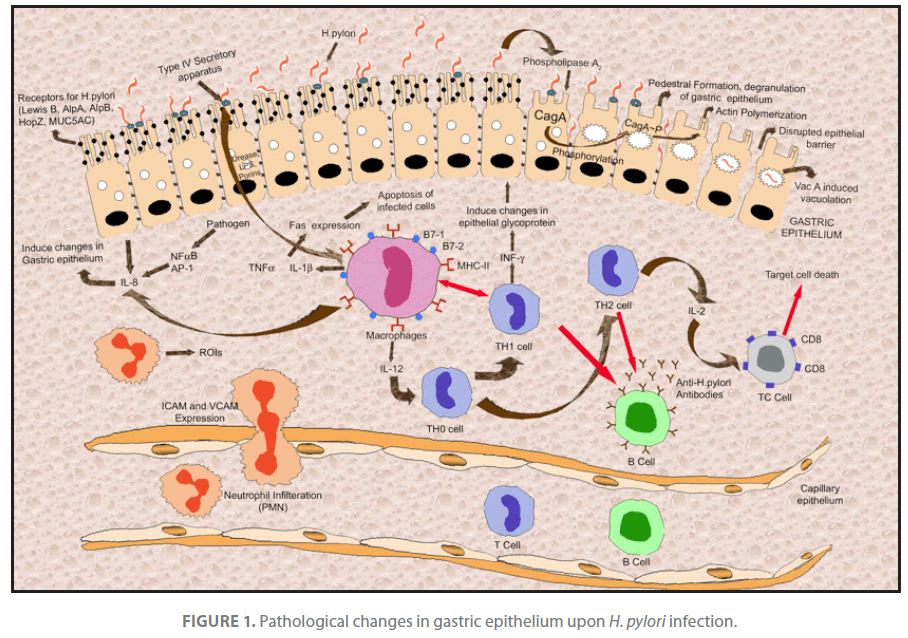
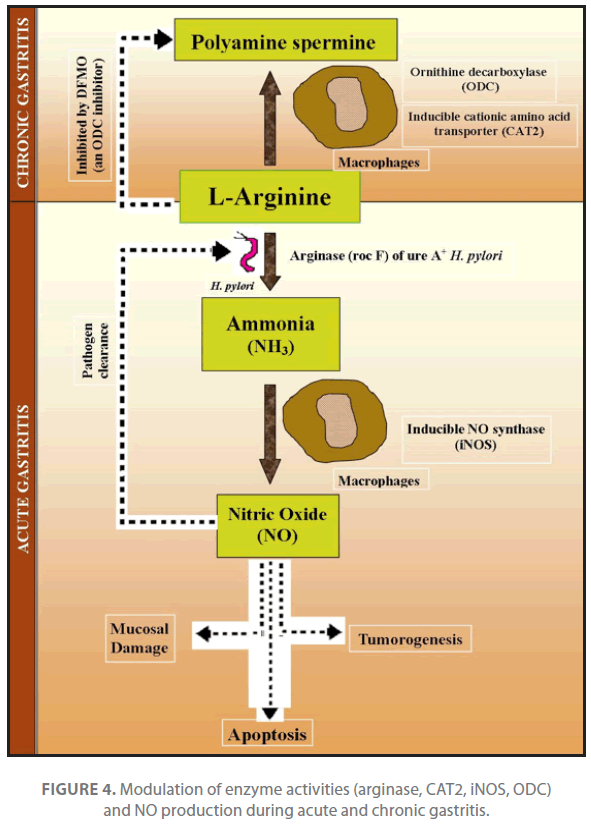
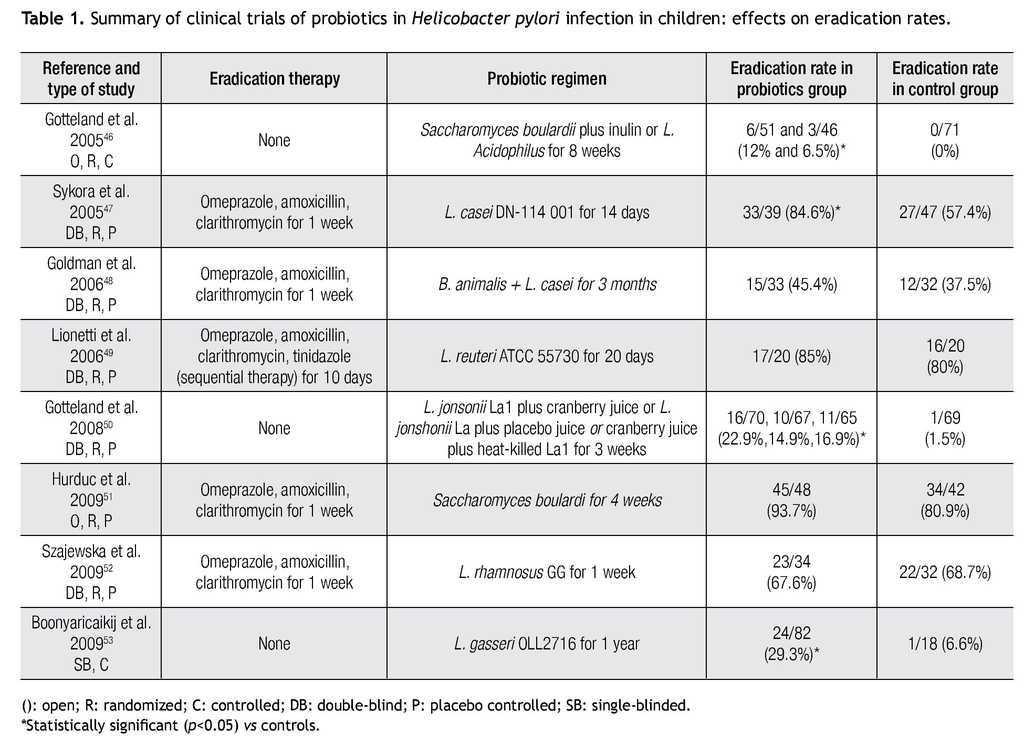
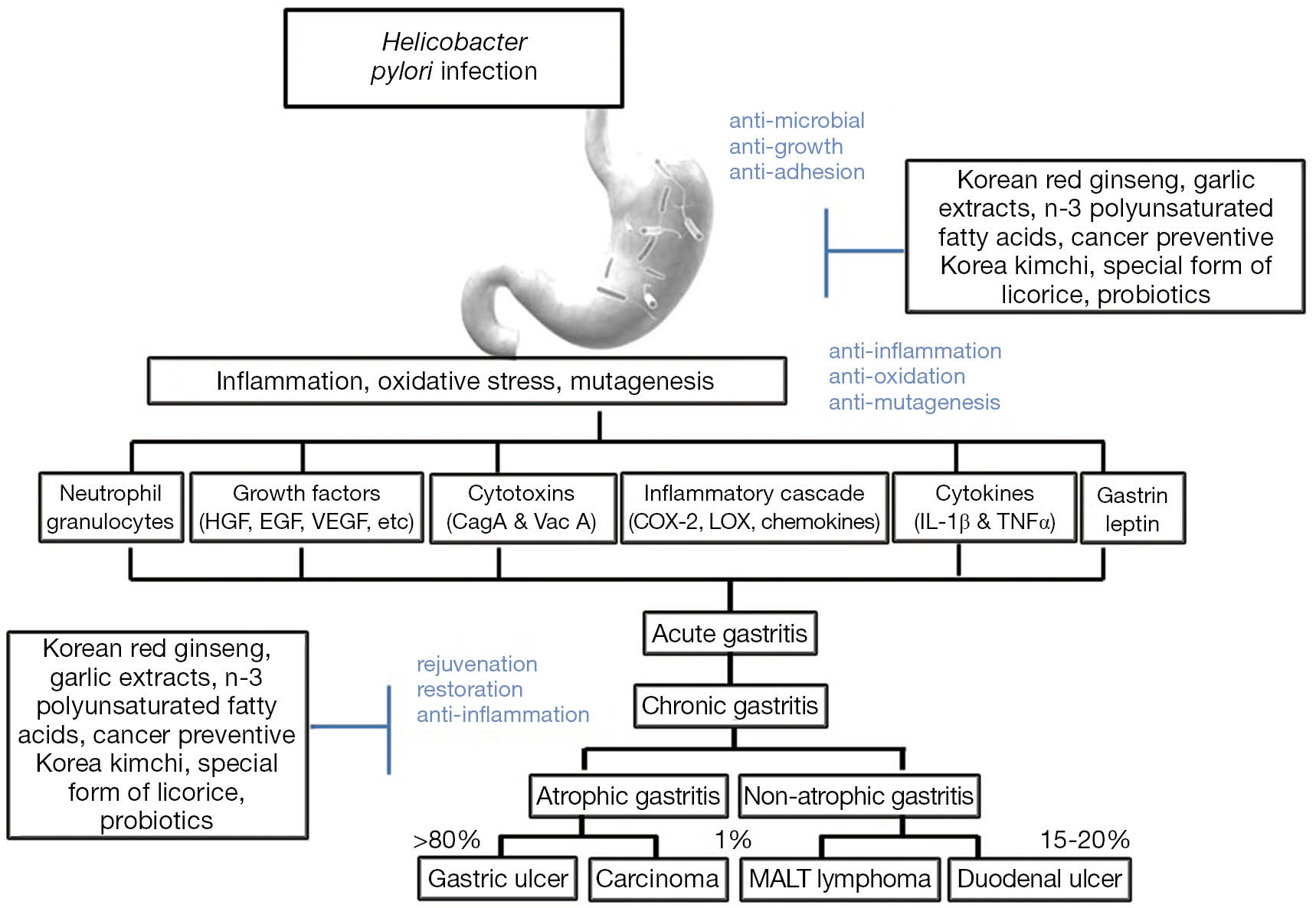
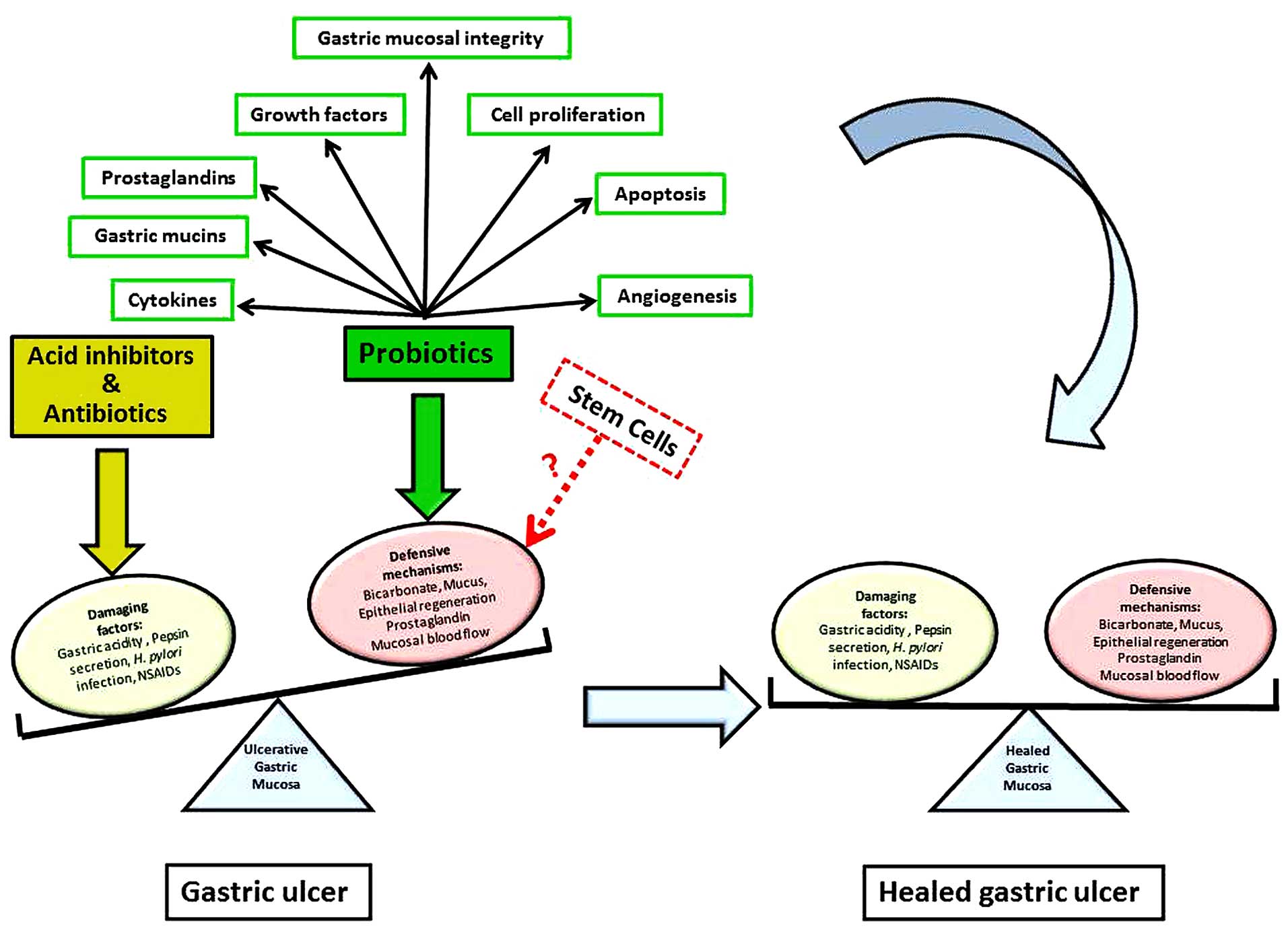
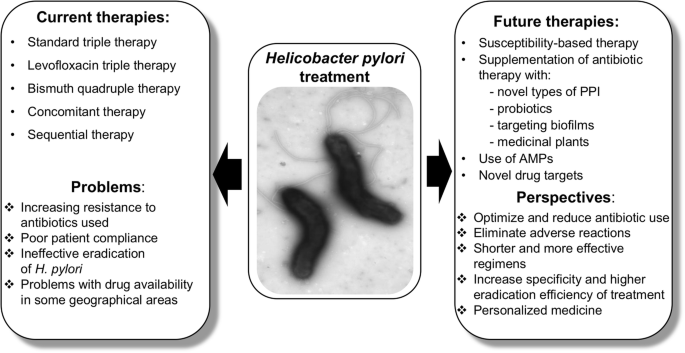
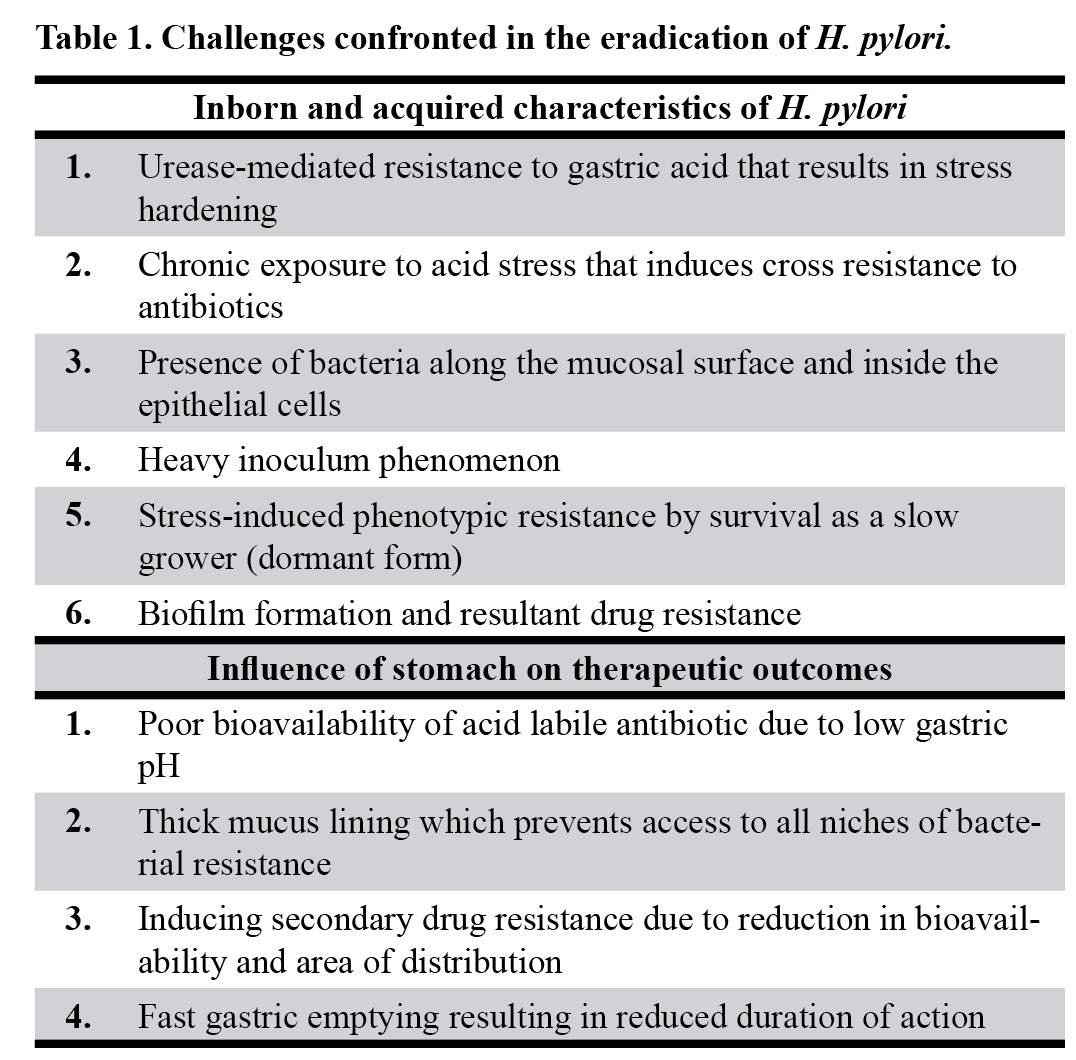
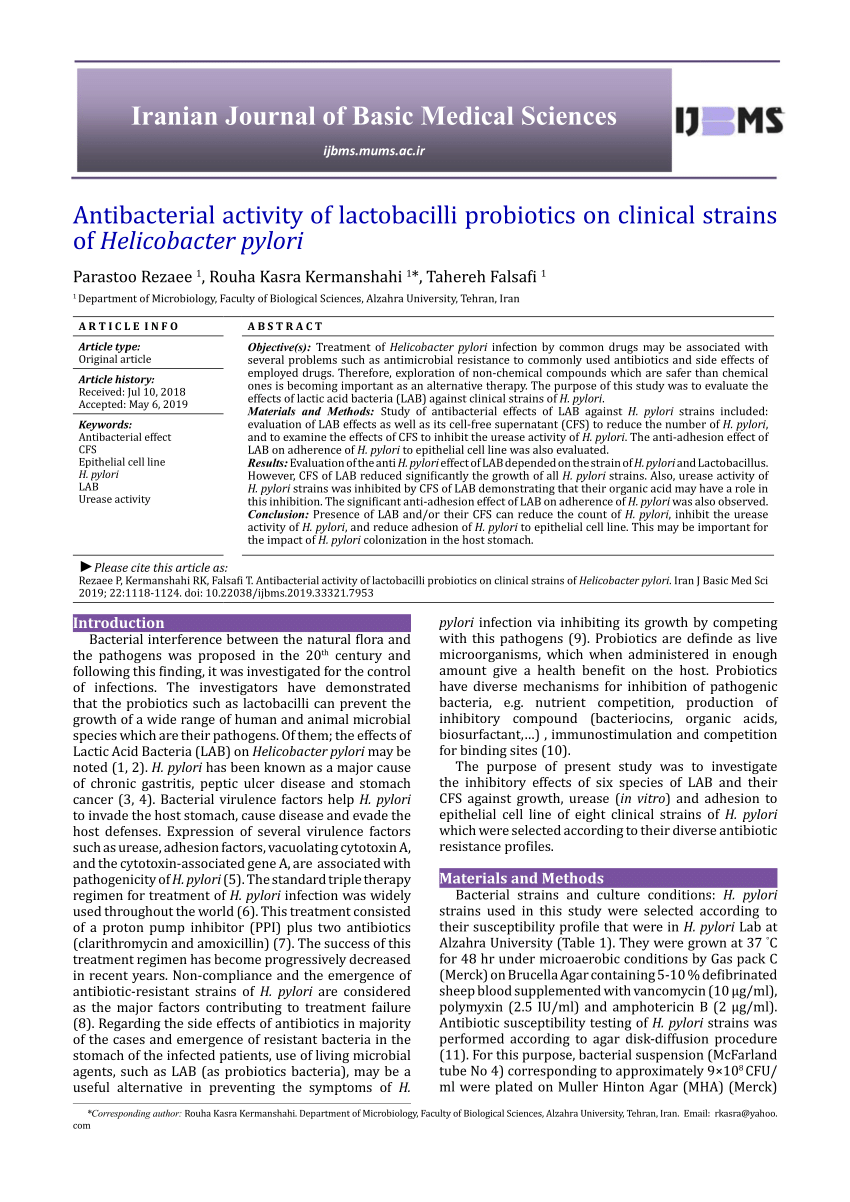
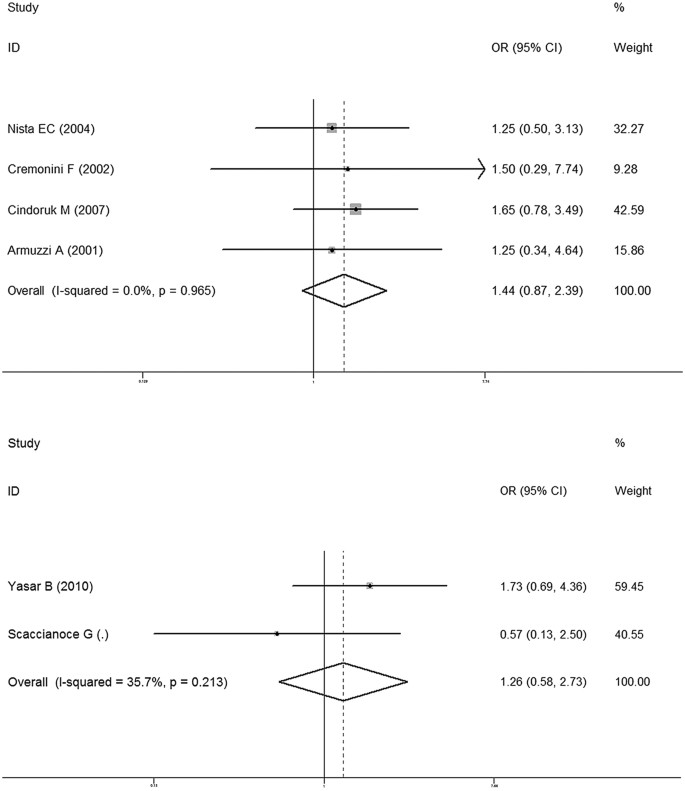
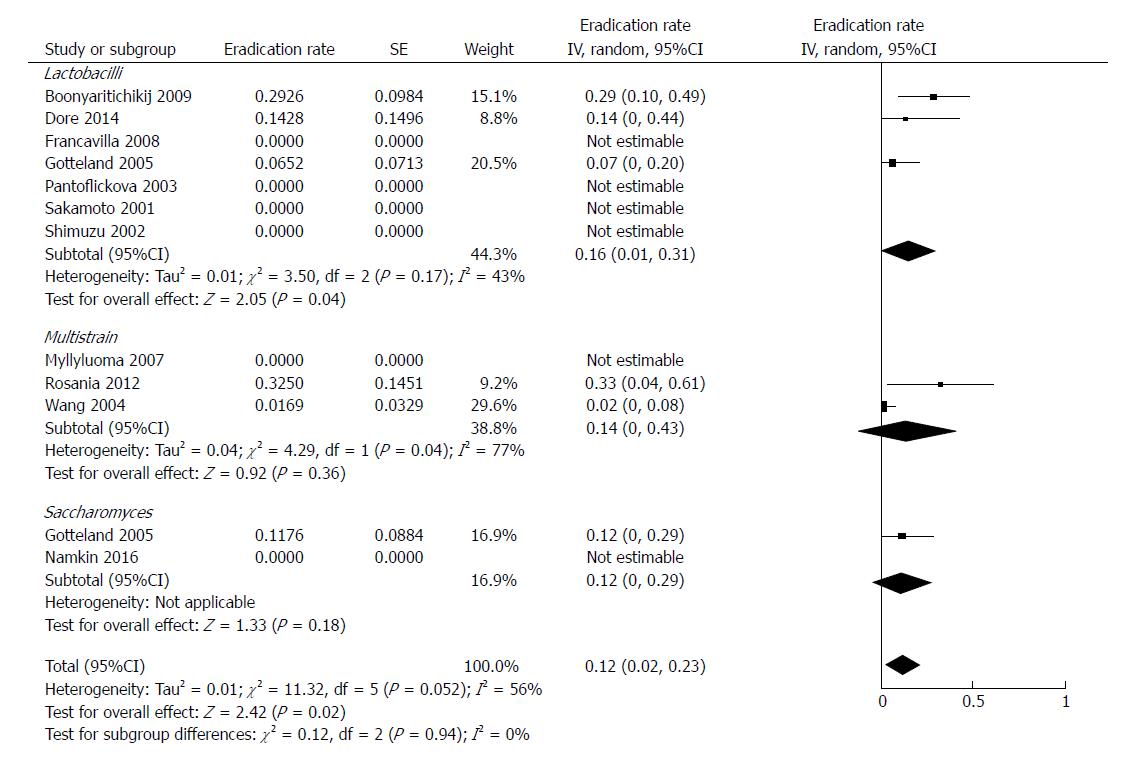
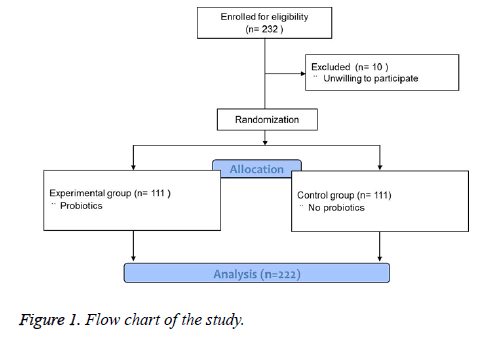
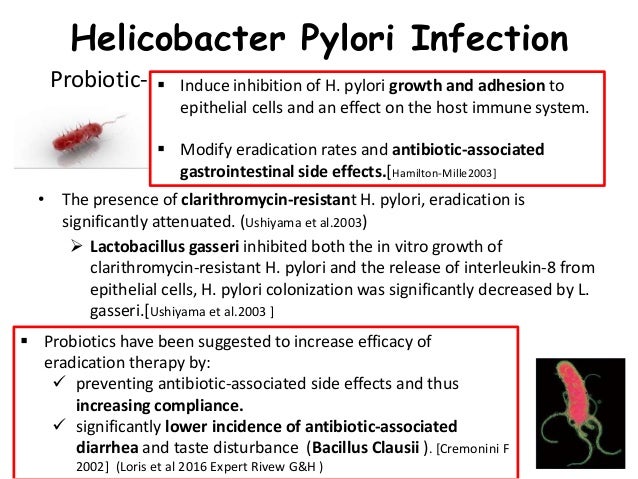
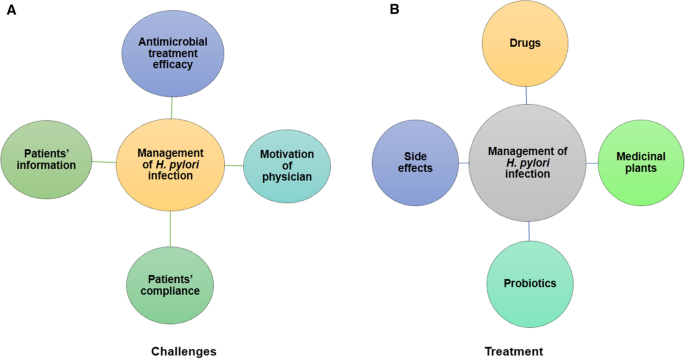
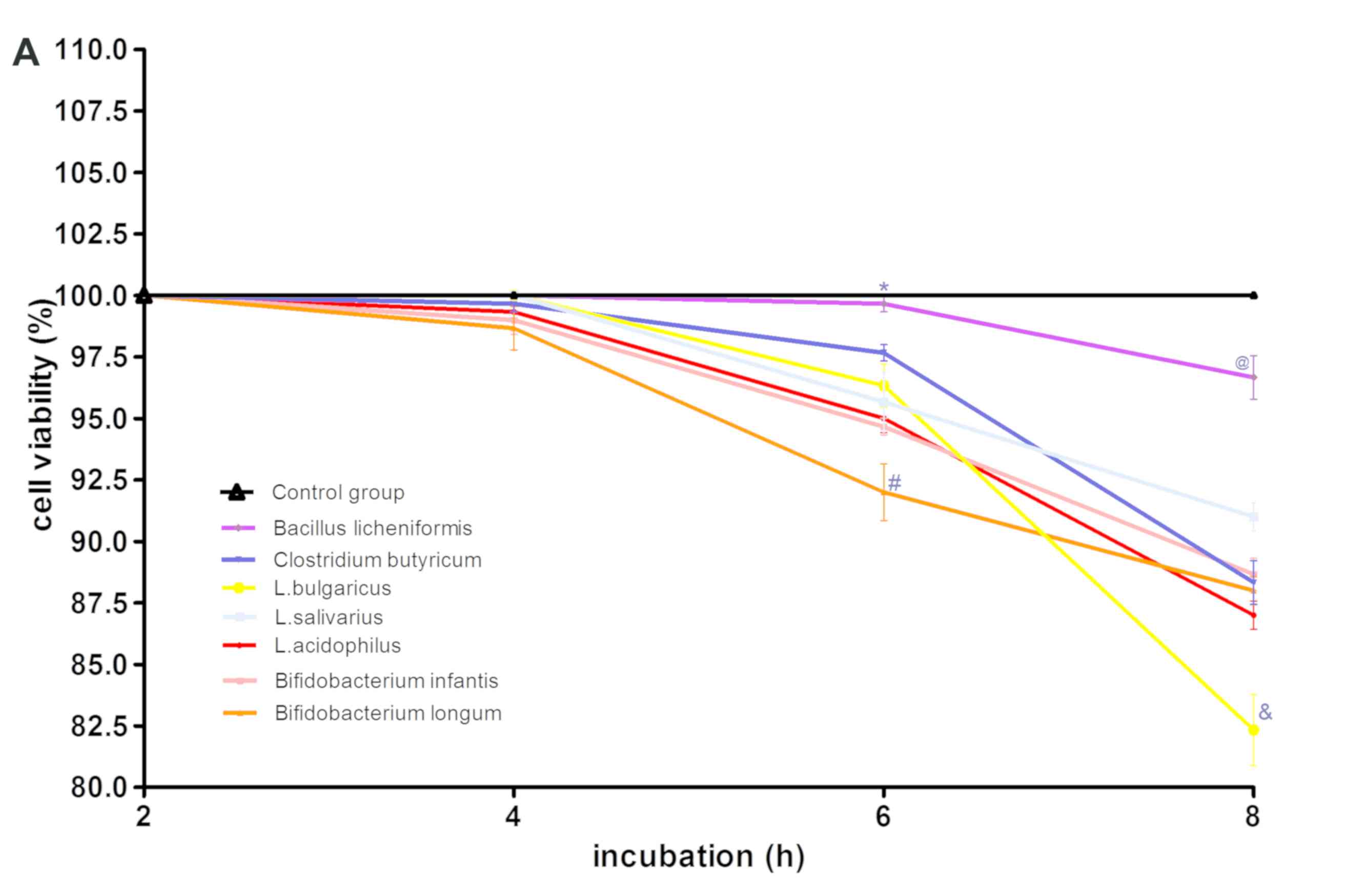
Are probiotics useful for therapy of Helicobacter pylori diseases? - ScienceDirectWarning: The NCBI website requires JavaScript to operate. Are the probiotics useful in the eradication of Helicobacter pylori? Correspondence to: Matjaž Homan, MD, PhD, University Children's Hospital, Bohoričeva 20, 1000 Ljubljana, Slovenia. Phone: + 386-15229276 Fax: + 386-15229206RestractHelicobacter pylori (H. pylori) is considered an etiological factor for the development of the disease of peptic ulcer, gastric adenocarcinoma and MALT lymphoma. Therapeutic schemes to eradicate bacteria are based on double antibiotic therapy and proton pump inhibitor. Despite many therapeutic improvements in the treatment of H. pylori eradication, it is still associated with a high rate of infection also in developed countries. Bacterial resistance and adverse events occur among the most common causes for the failure of anti-H. pylori treatment. Several studies have reported that certain probiotic strains may exhibit inhibitive activity against H. pylori bacteria. In addition, some probiotic strains can reduce the occurrence of side effects due to antibiotic therapy and, consequently, increase the rate of H. pylori eradication. The results of the prospective studies controlled by double-blind placebo suggest that specific probiotics, such as S. boulardii and L. johnsonni La1 may decrease the bacterial load, but not completely eradicate the H. pylori bacteria. In addition, it seems that supplementation with S. boulardii is a useful concomitant therapy in the standard treatment protocol H. pylori eradication and probably increases the eradication rate. L. reuteri is equally effective, but more positive studies are needed. Finally, the probiotic strains, such as S. boulardii, L. reuteri and L. GG, decrease the associated adverse gastrointestinal effects. Basic Council: Deficient eradication rates have been reported in the infected patients of Helicobacter pylori (H. pylori), which is mainly explained by the increase in bacterial resistance rates to antibiotics and the low compliance of these drugs. This situation needs the development of alternative treatment options for H. pylori infection in patients. The results of recent studies suggest that certain test strains complemented by standard eradication therapy decrease the frequency of gastrointestinal adverse effects and therefore increase eradication rates. HELICOBACTER PYLORIHelicobacter pylori (H. pylori) is a gram-negative microorganism. Since the original discovery of the Helicobacter genus, more than 20 species have been formally defined.[] Gastric mucosa is well protected against bacterial infection. After ingestion H. pylori must survive the bactericidal activity of gastric lumen and enter the layer of mucus. H. pylori is well suited to special conditions in the stomach. It possesses flagella, which allows the colonization of the gastric epithelium[]. In addition, the bacteria produces the urease enzyme, which hydrolyzes the urea in carbon dioxide and ammonia and elevates the pH in the environment of the bacteria. The enzyme activity is higher in low pH[]. Bacteria H. pylori usually causes chronic infection due to a complex balance between host factors and bacterial factors of virulence. Among several bacterial factors one of the main factors, which leads the Th17 inflammation, represents the prolyl cys secreted peptidil, trans-isomerase[]. In colonization and chronic infection the adherence of the bacteria to the gastric epithelium is also very important. Lipolysaccharide is a component of the bacterial wall consisted of a specific or polysaccharide chain, oligosaccharide and lipid A. The antigens similar to Lewis (Lex, Law, Lea, Leb) of H. pylori lipolysaccharide are also expressed in the epithelial cells of the gastric mucosa, so they probably play an important role in the cells About 5% of the H. pylori genome encodes external membrane proteins (OMP). WMOs are adhesins on the surface of the bacteria, which promote the union of epithelial cells in the stomach. The main WMP is the antigenous adherence of the blood group A (BabA), which means the binding of H. pylori to the antigen of the blood group of fucosylated Leb. Also mediate the union to the salivar mucin MUC5B, a proline-rich glycoprotein, and glycoprotein gp-340[]. The second most important WIPO is the adherence to the sialic acid (SabA) binding.[] Halfway the union of the bacteria to sialil-dimeric-Lex, to the salivar mucin MUC5B, and to salival glucoproteins such as MUC7 and zinc-glycoprotein[]. In gastric colonization, other WMOs such as AlpA, AlpB, HopZ and HomB are also involved. Therefore, the union of the tension of bacteria to gastric epithelial cells is also enabled with BabA2 and Saba adhesins. The H. pylori is very closely associated with the extracellular cells MUC5AC and epithelials that produce MUC5AC, therefore MUC5AC plays a role in the adherence of H. pylori to the gastric mucosa. The important receptor for bacteria is the Leb structure present in normal gastric tissue and MUC5AC is the most important carrier of Leb, with the attachment that is done through BabA[]. H. pylori infection remains one of the most common bacterial infections worldwide. H. pylori infection is very common in Eastern Europe, Africa and most Asian countries[]. In developed parts of the world prevalence has decreased and is less than 10% in children and less than 30% in adults.[] 20% of infected individuals develop symptomatic gastritis, gastric or duodenal ulcer, gastric adenocarcinoma and non-Hodgkin gastric lymphoma[]. H. pylori is also associated with iron deficiency anemia, idiopathic thrombocytopenic purpura and vitamin B12 deficiency[]. Several bacterial, host and environmental factors have been studied to determine the clinical outcome of H. pylori infection. Among the bacterial factors, the virulence genes are more important, and the severity of the disease related to H. pylori correlates with the presence of cagA, vacA s1m1 and genotypes babA2[,]. Chronic active gastritis can lead to precancer lesions such as gastric mucous atrophy and intestinal metaplasia, and finally to the development of gastric adenocarcinoma. The results of recent studies support the beneficial effect of H. pylori eradication on the prevention of gastric cancer, as well as on the regression of mucosa atrophy and intestinal metaplasia of gastric mucosa[]. Therefore, precancer gastric lesions require the rapid detection of H. pylori and the eradication of bacteria. It is suggested that H. pylori also have beneficial properties. Several meta studies and analysis showed an inverse relationship between H. pylori infection and the appearance of asthma[,]. The association was stronger for children than adults, but more prospective studies are needed to confirm the relationship mentioned above. In addition, H. pylori infection probably decreases the prevalence of obesity in children[]. The association between H. pylori infection and gastroesophageal reflux disease is still unclear. Although it has been previously suggested that the eradication of H. pylori may cause reflux disease, the existence of such an association was not recently confirmed.[] Standard eradication therapy consists of two antibiotics and a long-lasting proton pump inhibitor for 7-14 d. The percentage of treatment failures is increasing and the main cause of this is bacterial resistance to frequently prescribed antibiotics. The frequent use of claritromycin for respiratory tract infections has led to high rates of resistance to claritromycin []. Metronidazole resistance has less clinical impact. Metronidazole resistance can be overcome partially by increasing the dose and duration of the treatment. H. pylori resistance to metronidazole has been reported between 30% and 40%.[] Eradication levels used by standard triple therapy are between 60% and 80%, the last being considered as the minimum acceptable level according to Maastricht guidelines. Therefore, there is a great interest in developing new alternatives to eradication therapy, such as quadruple therapy or sequential therapy. Another possibility is to add the additional medication to the standard therapy protocol. Several studies have examined the potential influence of probiotics as supplements to standard therapy in the H. pylori eradication rate. In addition, probiotics were studied to reduce the frequency of side effects, as adverse events related to H. pylori therapy are an important factor that influences compliance. The overall rate of adverse events was 53.3% in a multicenter study[]. The most common adverse events reported are diarrhea, nausea and vomiting, which have significant physical and social impacts, and it has been shown that side effects were significantly associated with decreased compliance and failure of treatment.[] PROBIOTICS The definition of FAO/WHO probiotics is that probiotics are living microorganisms that when administered in appropriate amounts confer a health benefit on the host[]. The most used probiotics in humans are microorganisms belonging to the genus Bififobacterium, Lactobacillus, Saccharomyces and Bacillus[]. They are used as a unique species or multispecies preparation. The beneficial effects of probiotics seem to be specific to the tension and dose-dependent. Clinical studies of human probiotics are increasing rapidly. The beneficial effect of probiotics is already confirmed in diseases such as acute diarrhea, antibiotic-related diarrhea, functional gastrointestinal disorders, intestinal inflammatory disease, etc.[]. H. pylori infection is also a field in which there is a particular interest in using probiotics. The GASTRIC MICROBIOTALactobacillus species are acid resistant and are usually present in healthy gastric microbiota. Some strains may even adhere to gastric epithelial cells so that they can stay longer than other bacteria in the stomach.[] These have been confirmed in a study where it was possible to detect L. reuteri 55730 adhering to gastric epithelial cells of healthy volunteers a few hours after oral administration[]. Elliott et al[] have observed that in a gastric ulcer rat activates the local microbiota changed into gram-negative bacteria including E. coli while the Lactobacullus species almost disappeared. In the process of healing gastric mucosa, the population of Lactobacillus resurfaced and this process was accelerated by the administration of oral lactulosa. This study suggests that normal gastric microbiota participates in the maintenance of healthy mucosa. In addition, the oral intake of probiotics can reinforce the protective functions in the stomach. DIFERENT MECHANISMS OF ANALYCTERIAL ACTION Probiotics can inhibit H. pylori by several immunological and non-inmunological mechanisms. Probiotics are able to modify the immune response of the host. Neutrophils, lymphocytes, plasma cells and macrophages are involved in the inflammatory response to H. pylori. The consequences are higher levels of pro-inflammatory cytokines, such as IL-1β, IL-2, IL-6, IL-8 and tumor necrosis factor α in the gastric mucosa[]. Probiotics such as L. salivarius WB 1004 have reduced IL-8 secretion in vitro by gastric epithelial cells[]. It seems that at least in vitro L. acidophilus can improve gastric inflammation induced by H. pylori by inactivating the Smad7 and NFκB[]. In addition, Zhou et al[] showed that L. bulgaricus inhibited the activation of the TLR4 signaling pathway and the production IL-8 induced by H. pylori lipolysaccharide in SGC-7901 cells. Gastric inflammation can be controlled at some level by different strains of Lactobacilli by inactivating JAK2 through the JAK-STAT tracks and through a greater expression of the SOCS protein family.[] H. pylori also induces the humoral response of gastric mucosa, which can contribute to gastric mucosa damage. Lactobacilli was able to increase the local concentration of IgA and decrease specific antibodies anti H. pylori IgG in animal models[,] Among non-immunological mechanisms probiotics are able to influence bacterial growth by secreting antibacterial substances such as lactic acid, short-chain fatty acids, hydrogen peroxide, and spiral bacteriocin. Metabolites can decrease the number of bacteria[] Lactic acid probably has an additional effect on H. pylori by lowering pH and inhibiting urease[]. L. acidophilus CRL 639 secrete a autolysin, a proteinaceous compound released after cell lysis, which has some antibacterial activity[]. Substances, similar to isocoumarin antibiotics, are produced by B. subtilis and can also kill H. pylori bacteria[]. L. reuteri ATCC 55730 produces unique substance called reuterine that suppresses the growth of spiral bacteria[]. Mucins are high molecular weight glycoproteins that protect the gastric epithelium. Gastric surface mucin is decreased in infected patients, because H. pylori suppresses the expression of MUC5AC and MUC1 genes[]. It has been shown that the cepa plantarum 299v increases the expression of the MUC2 gene and that L. rhamnosus GG stimulates the expression of the MUC3 gene and the subsequent extracellular secretion of the mucin by the cultures of the colon cells[,]. Therefore, the ability of some probiotic strains to increase mucin production can protect the gastric mucous barrier against the adhesion of pathogenic bacteria such as H. pylori. The adherence of H. pylori to the host tissue is of vital importance for the colonization of the gastric mucosa[]. There are several proposed anti-adherence mechanisms of probiotics. L. reuteri and W. confuse are able to compete with the H. pylori strains for the adhesion sites. For example, the strains of L. reuteri, JCM 1081 and TM 105 inhibit the union of spiral bacteria to glylipid asialo-GMI receptors and sulfatide[]. In addition, Sakarya et al[] showed that S. boulardii contains neuraminidase activity, which eliminates the sialic acid linked to the α(2-3) surface, the ligand for H. pylori adhesion that binds sialic acid. POSSIBLE ROLE OF PROBIOTICS IN H. PYLORI TREATMENT The rate of eradication failure of more than 20% and the high percentage of adverse effects of antibiotic therapy are the main problems in standard eradication therapy protocols. In addition, the fulfillment of the lover due to adverse events results in increased antibiotic resistance of bacterial strains. Studies published to date suggest that probiotics can have a double role in fighting H. pylori infection. The frequency of gastrointestinal adverse events caused by antibiotic therapy decreases and the rate of eradication increases. Probiotics have been piloted as unique therapy in eradication protocols or as a therapeutic agent used concomitantly with standard eradication therapy. Probiotics as Unique Treatment in Treatment H. pylori The first positive results in vitro were published in 1989[]. Bhatia et al[] found that H. pylori growth in vitro washibied, if L. acidophilus was present in the culture. Michetti et al[] studied for the first time the effect of probiotics [L. acidophilus (La1)] on colonization H. pylori in humans. The study showed that the density of the bacterial load decreases in the probiotic group of asymptomatic patients, while the total eradication of H. pylori was not successful. Similarly, Wang et al[] revealed that after the intake of B. lactis Bb12 and L. acidophilus La5 in H. pylori infected adults a decrease in urea breathing test values was detected. The bacterial load was evaluated by the semi-quantative breathing test 13C-urea in subjects treated with L. johnsonii La1[], L. brevis CD2 lyophilized bacteria[], B. bifidum BF-1[], L. reuteri ATCC 55730[], L. gasseri OLL 2716[], and with significant respiratory probiotics Gotteland et al[] includes 182 asymptomatic children infected with H. pylori and divided into four groups: standard triple therapy group, S. boulardii and inulin symbiotic group, probiotic group L. acidophilus LB, or control group without any therapy. Statistically significant decreases were detected in the urea breathing test values in two groups: the standard triple group and the symbiotic group of inulina S. boulardii children. The authors concluded that S. boulardii can lower the bacterial load in the gastric mucosa of children infected with H. pylori bacteria. Surprisingly, in 12% of the children of the second group treated with S. boulardii and inulin H. pylori even eradication was successful. The same author conducted a randomized and double-blind study in 295 asymptomatic children infected with H. pylori[]. The study compared eradication rates after 3 wk therapy with (1) placebo/L. johnsonii La1 juice; (2) cranberry juice /L. johnsonii La1; (3) placebo/heat-qualified juice L. johnsonii La1; and (4) cranberry juice/heated juice L. johnsonii La1. Except for the placebo group the eradication rates were higher than 14% in all tested groups, but they do not statistically differ significantly from each other. Cruchet et al[] included 326 children infected in a similar study. The children were divided into five groups. They were treated for a month either with L. johnsonii La1 or L. paracasei ST11 alive or inactive. The fifth group was the control group. Statistically significant changes were observed in the 13C-urea respiratory test only in the group of pediatric patients treated with L. johnsonii La1 living probiotics. In conclusion, there are only some studies that evaluate the effect of probiotics as monotherapy in the H. pylori eradication rate. The results of the studies suggest that specific probiotics, such as S. boulardii and L. johnsonni La1 probably decrease the bacterial load, but do not completely remove the H. pylori bacteria. Probiotics such as adjuvant therapy in standard eradication protocols Several systematic reviews and metaanalysis have been published regarding the effect of probiotics as adjuvant therapy to the standard treatment of H. pylori infection[,]. The authors suggested that the supplementation of probiotics in general would likely increase the rate of eradication and reduce the frequency of adverse effects due to dual antibiotic therapy. However, the beneficial effects of probiotics seem to be specific to the strain, so collecting data on different strains in metaanalysis can result in misleading conclusions. With regard to this, a better approach is to unite data on the tension of individual probiotics and to perform a meta-analysis. Szajewska et al[] recently published a systematic review to assess the effects of supplements with S. boulardii to the standard triple therapy protocol on the H. pylori eradication rate. Five randomized controlled trials of good methodological quality involving 1307 patients were identified. Only 90 children were included. The daily dose of S. boulardii ranged between 500 mg and 1000 mg and the duration of therapy was 2-4 wk. Since four trials, complete data on eradication rates were available. In 80% of patients treated with boulardii S together with triple therapy, the eradication was confirmed by standard diagnostic tools. The control group detected an absolute eradication rate of 9 per cent mistress (71%, 324 of the 455 patients). The authors concluded that compared to placebo or without intervention, S. boulardii given along with triple therapy significantly increased the rate of eradication [relative risk (RR) = 1.13, 95%CI: 1.05-1.21]. The side endpoints of the same metaanalysis also determined the effect of S. boulardii on the adverse effects related to therapy. About 24.3 per cent of patients experienced adverse effects in the control group treated with triple therapy, compared to 12.9 per cent of patients in probiotic group. Thus, the significant difference was found between group S. boulardi and the control group regarding the risk of general adverse effects (five randomized control tests, n = 1305, RR = 0.46, 95% CI: 0.3-0.7). The authors also analyze the specific adverse effects data. With respect to epigastric pain, impairment of taste/dry mouth, nausea or abdominal/blocker gas, no significant difference was found between the studied groups. On the other hand, the risk of diarrhea-related therapy was statistically significantly lower in the probiotic group compared to the control group treated only with antibiotics and proton pump inhibitor (5.6% vs 12.2%, RR = 0.47, 95% CI: 0.32-0.69). The findings of metaanalysis were that the concomitant use of S. boulardii with triple therapy increases moderately H. eradication rates of pylori and decreases the adverse effects related to antibiotics, especially diarrhea. However, more recent studies published by Song et al[] and Zojaji et al[] did not confirm the positive impact of S. boulardii on the eradication rate. In the Song 991 H. pylori study infected patients were recruited. The patients of group A were treated only with two antibiotics and proton pump inhibitor, in group B S. boulardii was added for a month, and in group C the same regime was used and also the D-9601 mucoprotector agent derived from asiatic Artemisia was prescribed concomitantly. Curiously, the eradication rate was significantly higher in group B and C compared to group A only if the intent was made to treat the analysis (P = 0.003), while the difference in the rate of eradication of patients by protocol was not significant. The conclusion was that supplementation with S. boulardi could be effective in improving eradication rates by reducing adverse effects, thus contributing to the termination of eradication therapy. Zojaji et al[] included 160 adult patients. In the study protocol probiotic S. boulardii was added to clarithromycin, amoxicillin and omeprazole for two weeks. The study showed that probiotics decrease the frequency of adverse events due to antibiotic therapy, but did not increase the rate of H. pylori eradication. Tong et al[] systematically evaluated the effectiveness of supplementation with different probiotics in the increase of H. pylori eradication rates. In the publication they also made subanalisi for different probiotic preparations. In eight of fourteen randomized trials a strain of individual probiotics was used. In tree trials, the species of Lactobacillus were administered to standard eradication therapy[-]. However, the increase in the eradication rate of H. pylori in the Lactobacillus group was reported in only two studies published by Sýkora et al[] and Canducci et al[]. In general, in tree studies, eradication rates were 70% in control group and 84% in complemented probiotic group, which is a statistically significant difference (RR = 2.09, 95%CI: 1.28-3.41). In addition, this meta-analysis revealed that the addition of probiotics to standard eradication protocols reduces the adverse effects during treatment (25% vs 39%, RR = 0.44, 95%CI: 0.30-0.66). The positive impact on diarrhea and taste alteration was more prominent. The efficacy of L. GG in children with H. pylori infection was studied in a Polish trial[]. Of the 83 children tested, 34 children in a group of probiotics received L. GG 109 twice a day for a week with three-fold therapy. No significant difference was found in H. pylori eradication rates between probiotic and control group (RR = 0.985%CI: 0.7-1.4). This result is consistent with adult trials. Armuzzi et al[] included 60 asymptomatic patients infected in a prospective study in which patients were treated with rabeprazole, clarithromycin tinidazole and L. GG or with the same triple therapy and placebo. Diarrhea, nausea and alteration of taste were significantly reduced in the supplemental group L. GG (relative risk = 0.1 CI of 95%: 0.1 ± 0.9; relative risk = 0.1 ± 0.9; relative risk = 0.5; 95% CI: 0.2 ± 0.9, respectively). Another Italian study included 85 asymptomatic adults, and the conclusion of the study was that supplementation L. GG to standard therapy beneficially affects the adverse effects related to treatment[]. However, it seems that L. GG has no effect on eradication rates. Demonstration that L. reuteri ATCC 55730 is able to colonize the stomach and duodenum driven studies on the effect of this strain on H. pylori eradication rates and the frequency of side effects[]. In a recent study conducted in Italy, Ojetti et al[] recruited 90 patients in his study. The supplementation of L. reuteri was used concomitantly for 14 d with second-line therapy that received esomeprazole, levofloxacin and amoxicillin in patients infected with H. pylori. Probiotic supplementation increased the rate of eradication in treated patients (group 1: 36/45, 80%; group 2: 28/45 62%; P The use of commercial yogurt containing B. animalis and L. casei combined with conventional triple therapy was investigated in two studies. Sheu et al[] proved the effectiveness of this yogurt as adjuvant for triple treatment. The difference in the rates of eradication of H. pylori infection in two groups was statistically significant in favour of the probiotic group (73/80 vs 63/80, P Effect of pretreatment with L. gasseri OLL2716 on first-line eradication therapy was studied in a trial published by Deguchi et al[]. Approximately 229 infected patients were randomized into two groups, either a week of triple therapy (rabeprazol, claritromycin, amoxicillin) or the same therapy with addition of probiotics. Overall eradication was significantly better in the studied probiotic group [intention to treatment (P = 0.018)/by protocol (P = 0.0411)], but more prospective studies are needed to evaluate the role of L. gasseri OLL2716 in treatment in H. pylori infection. The beneficial effects of adding fermented milk products containing L. casei DN-114 001 to triple therapy on the rate of eradication of H. pylori infection in children were shown in a multicenter study of the Czech Republic[]. Eighty-six symptomatic children infected with H. pylori were randomized to receive omeprazole, amoxicillin, clarithromycin or the same regime with addition of probiotics for 7 d. The eradication rate was statistically significantly higher in the probiotic group (P = 0.0045). B. claussi has also been studied as a possible complement to standard therapy for the eradication of H. pylori, but the positive effect on the eradication rate was not confirmed[]. The characteristics of the important studies in which probiotics were used as adjuvant therapy for the treatment of eradication are presented in table .Table 1Probiotics as adjuvant therapy in eradication protocols Helicobacter pylori Ref.TerapiaStudy Eradication rate Adverse effects Eradication therapy (d)Probiotic therapy (d) No. H. pylori H. pylori + probiotic therapy H. Pylori therapy H. pylori + probiotic therapyH. pyloritherapyCindoruk et al[]PPI + AC (14)S. boulardii (14)124UBT44/62137/6214/62137/62Cremonini et al[]PPI + CT (7)S. boulardii (14)43UBT 17/203/21112/20Duman et al[] 45/4834/424/48113/42Song et al[]PPI + AC (7)S. boulardii (28)661UBT264/330237/33148/330163/331Zojaji et al[]PPI + AC (14)S. boulardii (14)160UBT75/8014/80129/80Canducci et al[] RUT23/3422/3218 GI (14)85UBT16/213/20112/20Ojetti et al[]PPI + ALL. reuteri (14)90UBT36/45127/4510/45126/45Lionetti et al[]uterI + ACT (10)L/2019 Emara et al[]PPI + AC (14)L. reuteri (28)70hist, RUT26/3523/3510/35124 Therefore, the eradication of H. pylori is a primary objective in symptomatic patients. Eradication rates reached by classical triple therapy were proton pump inhibitor and double antibiotic therapy are fairly low and range between 60% and 80%, due to resistance to antibiotics and moderate patient compliance. Gastrointestinal adverse events associated with antibiotics are the main cause of minor compliance. It was therefore proposed that probiotics be a useful complement to improve the eradication rate and reduce the frequency of adverse effects. So far, most of the different types of Lactobacillus and S. boulardii were tested. The above-mentioned probiotics probably decrease the bacterial load but do not eradicate completely H. pylori in the gastric mucosa, if used as monotherapy. On the contrary, some probiotics when added to triple classical therapy can increase eradication rates. There is a reasonable amount of evidence that supplementation with S. boulardii is a useful concomitant therapy in the standard H. pylori eradication treatment protocol and probably increases the rate of eradication. L. reuteri is also a good candidate for adjunctive therapy, but more positive studies are needed. The effect of other probiotic strains is less well described. Side effects, caused by double antibiotic therapy, can be reduced with probiotics. Probiotic strains, such as S. boulardii, L. reuteri and L. GG, decrease the adverse effects associated with gastrointestinal antibiotics, especially diarrhea. The Maastricht IV/Florence Consensus Report suggests that certain probiotics and prebiotics show promising results such as adjuvant treatment to reduce side effects[]. FootnotesConflict-of-interest statement: Authors have no conflict of interest to declare. Open-Access: This article is an open access article that was selected by an internal editor and reviewed by external experts. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0), which allows others to distribute, remix, adapt, build on this non-commercial work, and license its derivative works in different terms, provided that the original work is duly cited and the use is not commercial. See: http://creativecommons.org/licenses/by-nc/4.0/Peer-review initiated: 3 March 2015 First decision: 30 March 2015 Press article: 2 September 2015P- Comment: D'Elios MM, Eren B, Malnick S, Sakarya S- Editor: Yu J L- Editor: A E- Editor: Wang CHReferencesFormats:Share , 8600 Rockville Pike, Bethesda MD, 20894 USA
Could Probiotics Be the Answer for Helicobacter pylori (H. pylori) Inf - Natren, Inc.

Are probiotics useful for therapy of Helicobacter pylori diseases? - ScienceDirect

Mechanisms of antagonism of probiotics against H. pylori | Download Scientific Diagram

H pylori Probiotics, and Treatment Success
Alternative Treatments for Chronic Gastritis Caused by H. pylori Infection - microbewiki

96% eradication rate: 14-day probiotic and antibiotic therapy effective in overcoming H. pylori in Thai population
Frontiers | The Probiotic Lactobacillus rhamnosus for Alleviation of Helicobacter pylori-Associated Gastric Pathology in East Africa | Microbiology
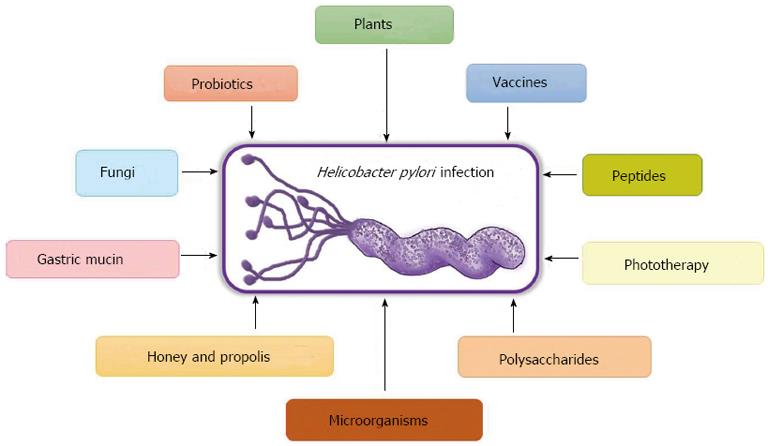
Exploring alternative treatments for Helicobacter pylori infection

Schematic presentation of possible mechanisms of probiotics to... | Download Scientific Diagram
Helicobacter pylori infection: efficacy of probiotics and role of genome wide association studies | Insight Medical Publishing
PROBIOTIC SCIENCE on Twitter: "#LG21, a #probiotics strain specialized in the use for the gastric diseases such as H. pylori infection and functional dyspepsia https://t.co/bdlHJZrMSW #IPC2018… https://t.co/axIbKOjgRG"

Lactoflor Helico Protect Probiotic with PYLOPASS

Helicobacter pylori and Probiotics | My Gut Matters
Helicobacter pylori infection: efficacy of probiotics and role of genome wide association studies | Insight Medical Publishing

Probiotics for H. Pylori - Balance ONE

H. pylori Natural Treatments: What it is & How to Get Rid of It - Dr. Axe
A new systematic review and meta-analysis explores the role of probiotics in Helicobacter pylori eradication therapy - Gut Microbiota for Health
![5 BEST Probiotics for H. Pylori - [REVERSE] H. Pylori 5 BEST Probiotics for H. Pylori - [REVERSE] H. Pylori](https://probioticsbeauty.com/wp-content/uploads/2020/04/best-probiotic-for-h-pylori-1024x536.jpg)
5 BEST Probiotics for H. Pylori - [REVERSE] H. Pylori
Probiotics and Helicobacter pylori infection | Medicina Universitaria
Dietary, non-microbial intervention to prevent Helicobacter pylori -associated gastric diseases - Han - Annals of Translational Medicine
Potential role of probiotics in the management of gastric ulcer (Review)

Helicobacter pylori and Probiotics | My Gut Matters
Helicobacter pylori treatment in the post-antibiotics era—searching for new drug targets | SpringerLink

Amazon.com: Lactoflor Helico Protect Probiotic with PYLOPASS which counteracts The Helicobacter Pylori Bacteria + Zinc-L-Carnosine: Health & Personal Care
![PDF] Effects of Probiotics and Prebiotics Helicobacter pylori and Probiotics 1 , 2 | Semantic Scholar PDF] Effects of Probiotics and Prebiotics Helicobacter pylori and Probiotics 1 , 2 | Semantic Scholar](https://d3i71xaburhd42.cloudfront.net/d48cd6da21f3685255cc0b5cfcad6d14991ce7ce/2-Table1-1.png)
PDF] Effects of Probiotics and Prebiotics Helicobacter pylori and Probiotics 1 , 2 | Semantic Scholar

Probiotics and Helicobacter pylori: Supplementation increases eradication speed and decreases side effects

Effectiveness of Probiotic strains in Helicobacter pylori eradication from stomach
Gastric Microenvironment Enables Persistence of Helicobacter pylori: a Physician's Combat Towards Eradication and Directions for the Future — Journal of Young Investigators

H. pylori: Natural Treatments and More
PDF) Antibacterial activity of lactobacilli probiotics on clinical strains of Helicobacter pylori
Probiotic supplementation does not improve eradication rate of Helicobacter pylori infection compared to placebo based on standard therapy: a meta-analysis | Scientific Reports

Tame the pylori burn with a probiotic fire-fighter
Probiotic monotherapy and Helicobacter pylori eradication: A systematic review with pooled-data analysis
Pylopass Eliminates H. pylori with Confidence. Trademarked L. reuteri
Probiotics improved the effectiveness and safety of the quadruple Helicobacter pylori eradication therapy

Role of Probiotics in Prophylaxis of Helicobacter pylori Infection | Bentham Science

Helicobacter pylori and Probiotics - Journal of Nutrition - American ...
Probiotics final 2
Helicobacter pylori: Perturbation and restoration of gut microbiome | SpringerLink
Probiotic effect on Helicobacter pylori attachment and inhibition of inflammation in human gastric epithelial cells
Posting Komentar untuk "h pylori and probiotics"